Edaravone in Australia: what it means for New Zealanders living with MND
Research, Treatments
9 May 2025

A treatment for motor neurone disease (MND) has been newly added to Australia’s Pharmaceutical Benefits Scheme (PBS), making it publicly funded there for the first time. The drug, edaravone (brand name Radicava), is now available to eligible Australians.
It is not registered in Europe or the UK after questions were raised about its effectiveness, and the registration application was withdrawn.
What is edaravone?
Edaravone is a treatment for amyotrophic lateral sclerosis (ALS) that has been available in the United States since 2017 as an intravenous infusion and, more recently, as a liquid taken by mouth or through a feeding tube. In the first month of treatment, infusions are given every day for 14 consecutive days. In subsequent months, this reduces to 10 infusions in a 14-day period followed by 14 days of no treatment. Each infusion takes about an hour. Edaravone is thought to slow the decline in physical function experienced by people with MND, although clinical trials have produced mixed results.
A 2022 European study (ADORE trial, conducted by Ferrer) found no measurable benefit, prompting the drug’s manufacturer, Mitsubishi Tanabe, to publicly distance itself from the findings. The company stated the trial differed significantly from its own clinical studies. Still, the conflicting data has added to international caution around the drug’s broader effectiveness.
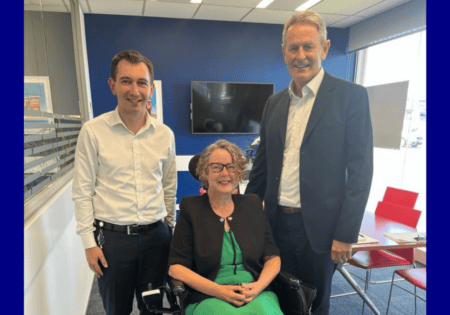
Neurologist Dr James Cleland, our Honorary Medical Advisor, has closely followed the global discourse around Radicava. While noting its recent listing on Australia’s PBS, he believes its mixed evidence base warrants caution.
“In the MND research and clinical spheres, we are always excited by the entry of new treatments for MND. However, we must carefully balance this enthusiasm with a careful assessment of the data in relation to effectiveness, practicality, and, of course, cost.
“While Radicava adds to the list of effective treatments, it is not highly efficacious, can be difficult and expensive to administer, and is therefore appropriate to be cautious about highly recommending this treatment.”
Dr Cleland also points to a broader issue: the ongoing focus on pharmacological solutions can sometimes eclipse the proven benefits of coordinated multidisciplinary care — a model that already offers meaningful outcomes for people with MND. Riluzole, which is funded in NZ, has been proven to modestly increase survival. Using bipap for breathing when needed, and maintaining body weight (including using a feeding tube if needed) are also beneficial for survival.
At Motor Neurone Disease NZ, we welcome robust, independent evaluation of any treatment that shows potential benefit. However, we remain focused on improving access to the most consistently beneficial support available now: equitable, coordinated multidisciplinary care.
The most effective support we already have
There is strong international evidence (Cochrane review, RACGP article) that access to multidisciplinary services — including neurologists, MND nurse specialists, speech-language therapists, occupational therapists, dietitians, physiotherapists, and others — leads to better outcomes, improved quality of life, and increased survival.
And yet, across Aotearoa, that kind of coordinated support remains uneven. People in some areas face delays, disconnected services, and a shortage of specialist input. Geography, funding, and workforce pressures all contribute to a system that can feel fragmented and hard to navigate.
As Dr. Cleland emphasises, the most equitable and effective path forward is to strengthen the care systems we already know work—not just to chase the promise of new medications.
Making time count
Helping people make time count is at the heart of what we do. From diagnosis onwards, we offer trusted information, practical support, and a compassionate presence for those affected by MND. We also advocate for better care, more investment, and smarter systems that truly serve the needs of our community.
Earlier this year, we conducted the most comprehensive national survey of the MND community ever undertaken in New Zealand, led by Dr Natalie Gauld. We invited people living with MND, carers, families, and healthcare professionals to share their experiences — with the aim of better understanding what matters most, and where support systems need to evolve.
This work will help inform how we advocate for more equitable access to multidisciplinary care — a proven approach that remains out of reach for too many. It provides a foundation for future conversations with decision-makers and ensures our efforts remain grounded in the real experiences of those living with and affected by the disease.
While pharmaceutical developments will continue to emerge, the most meaningful support we can offer right now is access to coordinated multidisciplinary care — support that helps people navigate the challenges of MND with greater dignity, connection, and quality of life.