Augmentative and Alternative Communication Awareness Month
Education, Living with MND
14 October 2024

October is International AAC Awareness Month, dedicated to raising awareness of augmentative and alternative communication (AAC), celebrate people who use AAC to communicate, and share the latest tools and technologies in AAC.
What is AAC?
AAC encompasses a wide range of communication tools and systems that people use to express their thoughts, needs, wants, and ideas.
These can include facial expressions, gestures, speech cards, eye gaze, and communication devices like tablets with language software.
AAC helps bridge the gap between communication challenges and participation in daily life.
AAC and Motor Neurone Disease
AAC is particularly relevant to the MND community, as some people with MND have speech deterioration and may communicate differently.
AAC helps to keep you safer – by ensuring others clearly know what you want or need, without a need to guess. This means decisions are made by you, and not by others. It is also reassuring for your family and support networks to know what it is you really want.
“Sometimes when people with communication difficulties (e.g. unclear, slurred speech) say something to someone – the person you are communicating with doesn't understand what it is you're trying to say, and they are uncomfortable telling you that they don't understand – so theyjust agree or nod. No one benefits from this, both feel unsure and unfortunately this means YOUR idea, your opinion, your want, your need is not being heard – it limits the opportunity for a conversation. And conversations are so important to relationships. Conversations can be had by computer or writing what you want – it just takes a bit longer – learning to be patient is a wonderful skill for all of us!”
Jeanette, MND NZ Support Advisor
AAC Tools and Systems for MND
There is a range of low – and high – tech AAC available to support speech deterioration:
- Communication boards, speech cards, and writing tablets
MND NZ has some basic speech cards , and some people create their own. Communication boards such as boogie boards and writing tablets can be used with just a finger if holding a stylus is tricky. Some people find writing is faster and more familiar than key pressing.
“Tech isn’t for everyone. I have known several people who have preferred to use a writing tablet or boogie board. One chap bought several boogie boards of A5 size. He had good hand strength and was able to write. He taped a hook onto each one so that he could attach it to his belt or belt loops and have it on hand wherever he went.”
Sally, MND NZ Support Advisor
- Speech generating devices
This technology creates spoken words.
Voice banking is the recording of your natural voice while it is still natural and strong, for the possible eventuality of losing your speech. You can voice bank on a mobile phone, computer, or digital voice recorder. As long as the recordings are produced in MP3 format, they can be used later within a speech generating device.
You can also use one of several online services to record yourself speaking a set of sentences into computer software. The software then takes these sentences, breaks them down into parts and uses these to create a synthetic voice which can speak anything, not just the sentences you recorded. The synthetic voice should sound somewhat like your natural voice but does depend on the quality of the recordings and the clarity of your speech at the time of recording.
Talklink Trust (Wahanga Tū Kōrero) are specialists in the area of AAC and can provide guidance on your voice banking journey. You do not have to refer to Talklink for voice banking. Talklink have put together a variety of resources, including videos and a comparison table of the different voice banking services, here.
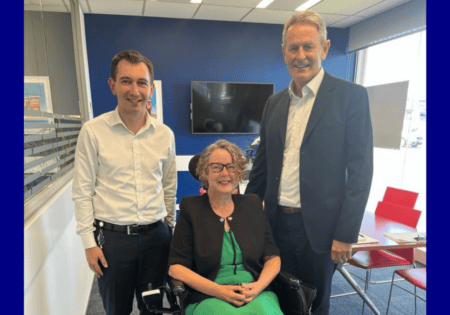
You can also watch a video of our own Natalie Gauld and Chris Kemp talking about their experience with voice banking, here.
The Space of Silence: supporting a person with speech difficulties
We asked our Support Advisors to share their tips for navigating communication and MND speech challenges:
“Learn to become comfortable with the often-uncomfortable space of silence. While the person with MND speaks with their dysarthric voice or uses any form of alternative communication, allow time, remain engaged while the pwmnd processes what has been said, formulates their response and communicates back to you and the wider group. Please avoid filling the waiting silence with carrying on the conversation or starting something new with the person or others. Like tramping- go at the pace of the slowest member of the team.”
“Negotiate with who you’re having a conversation with – if they are using a typing assisted communication – would they like you to guess at their words or wait until they fully type the word/sentence out?”
“Own what you don’t understand. It is ok to be honest and admit that you didn’t understand what a person with dysarthria has said or their mode of assisted communication. People appreciate honesty rather than you guess and respond out of context. It is often appreciated when you acknowledge how important what they said to you is and try again. Using “I“ statements rather than “you” is helpful.”
“Workplaces supporting staff with MND: email the person with questions prior to a meeting so they can prepare their responses beforehand.”
“When I do presentations at rest homes for the staff, I always get one of the staff members to sit in a chair and instruct them to not talk, but to only nod ‘yes' or ‘no' to my questions. I will then start off with a ‘yes' or ‘no' question such as “would you like breakfast”? This is easy for them, and I quickly get a ‘yes' nod of the head. I then ask, “so what would you like for breakfast”? This question clearly needs to be answered verbally and because I have instructed the staff member not to talk, they then quickly realise how difficult it is for their MND patient to answer questions from staff, if they are not using the correct form of communication. I find by putting staff members in role-play situations at the rest home, helps them to better understand what their MND patients are going through.”