2018 Research Update: MND Research News
Research
25 July 2018
A summary of research from the 2018 Australasian MND Symposium.
This information will be of interest to people with MND, their carers and health professionals.
Below is a broad update about developments in research towards a cure and understanding the causes of MND, including a proposed staging system for MND (similar to that used for cancer) and an important update to our understanding of riluzole.
- For an easier to read format, please click here for a PDF of the text below.
“It’s a very exciting time to be involved in MND research. There’s a lot of hope and positivity”
– Prof Matthew Kiernan, Bushell Chair of Neurology, Sydney Medical School.“I’m really optimistic for the future for the next 5 to 15 years. It will lead to a cure.”
– Prof Paul Talman, director, Australian MND Registry.“I’m much more optimistic than I was 10 years ago. There are more academic neurologists working on this in the UK than would be justified if you simply took the incidence of the disease. Researchers are intensely interested in MND, because it’s an interesting problem. For lots of us, it’s also a tractable problem – it’s not impossible, it’s just difficult.”
– Prof Kevin Talbot, Head of Clinical Neurology, Univeristy of Oxford UK.“There are lots of cracks in the wall of the dam. It will crack, and of all the neurological diseases MND will crack first.” – speaker from Australian Clinical Trials
“The rate of progress in recent years is very exciting.” – Lucie Brujin, Chief Scientist, ALS Association
Overview
What we know:
- 4-5 million people now alive today will die from ALS.
- MND is a disease of two motor systems (upper and lower), with enormous heterogeneity (variety).
- Multiple triggers.
- Focal onset typical, evolving to global dysfunction.
- Long pre-clinical period.
- Several competing ideas as to progression of disease.
- Some fundamental principles about ALS are not agreed among experts.
Barriers to effective treatment: late diagnosis, high level of biological complexity, poorly predictive preclinical models.
We are in a phase of defining the disease. Trying to break down the disease, moving into the era of precision/personalised medicine.
Those with familial MND will eventually be treated with therapies targeting DNA. DNA treatments (eg ASOs, CRISPR) for MND are 5-10 years away (due to technical issues) – but it will happen.
Those with sporadic MND will eventually be treated with precision medicine. Sporadic MND will be redefined, stratefied into sub-types according to biomarkers (eg fast and slow progressors) so that treatment can be personalised. Precision medicine is based on understanding the disease mechanisms, biomarker screening, staging model and individual responses to treatment.
What causes MND? Why me?
Prof Ammar Al-Chalabi
Prof of Neurology and Complex Disease Genetics, Director King’s MND Care and Research Centre, UK
Prof Ammar Al-Chalabi is one of the world’s top researchers in MND.
The differentiation between familial and sporadic ALS is not as clear as once thought. There is no consistent definition of familial ALS. All fALS genes have been found in people with sporadic ALS.
We now know of 25 risk genes for MND. At the rate of discovery, in four years we will have found 50. (Each of these risk factors increase your risk of MND by 5-10%.)
60% of whether you get MND is genetic factors, 40% is environmental.
It’s much harder to identify environmental risk factors than to find genetic risks. Environmental risk factors that many (not all) studies have agreed on are: smoking, trauma (eg broken bone, surgery), diesel fumes, exercise, being a war veteran.
Taking lessons learnt in cancer, he describes MND as a multistep process where genetic risk & environmental factors accumulate over time until threshold of disease is reached.
Studies that map MND against age in the UK, Netherlands, Italy, Ireland and Scotland have all shown that this is very likely and about 6 steps are required for MND to happen. Read his Nature article here
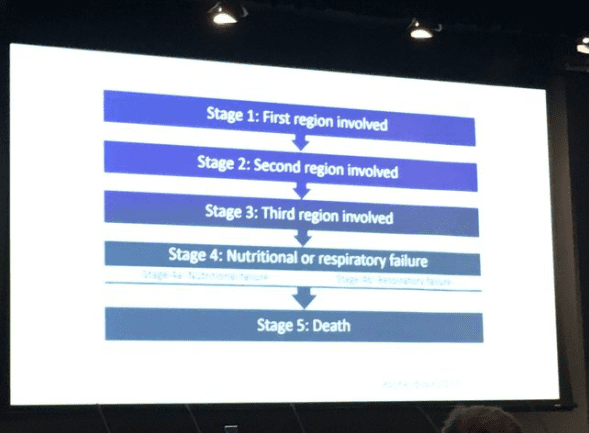
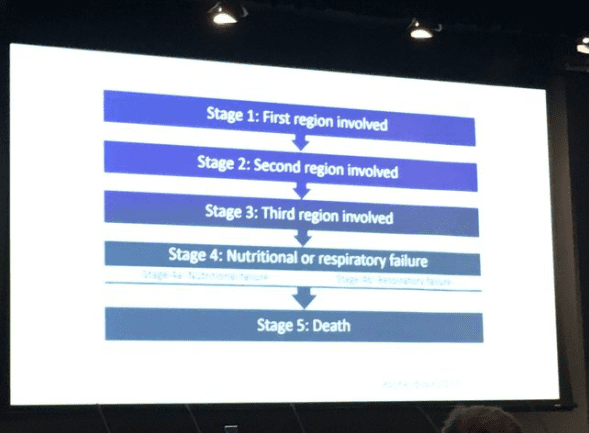
He proposes a staging system for MND, similar to the way cancer is defined in stages. See image, right.
This approach lets us look at which stage rilzole treats. It appears that it may have no effect in the middle stages. Riluzole prolongs the final stage of MND. It may also prolong the first stage but we have no data so this effect is unknown.
We highly recommend watching this full presentation:


Why Haven’t We Found a Cure Yet?
Prof Kevin Talbot
Head of Clinical Neurology, University of Oxford, UK
MND is complex but there is cause for optimism.
MND is not one ‘disease’, it’s a spectrum of things converging on one system – the cortico motorneuronal system.
We have tried drugs in 100 clinical trials or more. Incredibly expensive, wasteful, not working. If we carry on like this we will fail.
Need to get better models that reflect patients eg stem cells.
Need biomarkers.
Need earlier diagnosis.
Genetic studies give us a better idea of the pathways that should be targeted by drugs, including common pathways between genetic and sporadic MND.
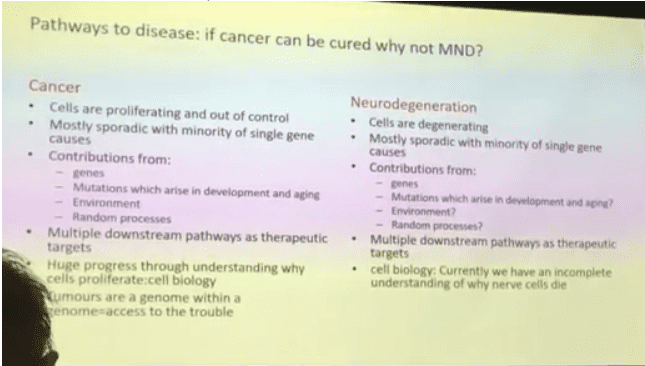
If cancer can be cured, why not MND? (See image, right.)
Biomarkers could stratify people into fast and slow progressors, predict regional spread.
Those with familial MND will eventually be treated therapies targeting DNA, and those with sporadic MND will be redefined according to sub-types so that treatment can be personalised.
DNA treatments (eg ASOs, CRISPR) for MND are 5-10 years away – technical issues – but it will happen.
Precision medicine will complement evidence based medicine.
Studies in pre-symptomatic gene carriers are essential.
Reason for optimism = exponential increase in our knowledge of basic mechanisms of MND. Increasing at an extraordinary rate, esp in last 2 or 3 years.
Highly recommend watching this full presentation:

MND in Australia
The Hon Greg Hunt MP
Australian Federal Health Minister
The rate of MND diagnoses has doubled in the last 20 years in Australia. There are now over 2000 people living with MND in Australia.
There is $31.7 million available to MND research in Australia (incl Medical Research Future Fund, Pharmaceutical Benefits Scheme). This is split between:
- primary research into cause of MND
- bringing young researchers through clinical fellowships
- pre-clinical trials
Mr Hunt said Australia’s research institutions rival Boston and Cambridge in skills and capacity. Australia is currently running 19 clinical trials related to neurology.
He also acknowledged that mental health in MND is important – it’s not just a physical challenge, it’s a mental one.
This raised some questions for MND NZ:
- Would any NZ Minister be that clued up on MND research?
- What (if any) NZ Govt funding is available for MND research?
- Should we extend MND NZ’s definition of research to include Australian research?
Prof Matthew Kiernan
Bushell Chair of Neurology, Sydney Medical School, Australia
It’s a very exciting time to be involved in MND research. There’s a lot of hope and positivity.
Australia and New Zealand are part of PACTALS, the Asia-Pacific consortium for MND/ALS research. The region includes 55-60% of the world’s population so there is huge potential for research here.
Being part of an international clinical trials network is also very important – it helps attract international pharma to Australia. There are multiple trials planned in Australia that involve international collaboration.
Some important areas of research:
- looking at HIV therapies as an anti-inflammatory approach to MND.
- the need to incorporate a biomarker arm into all clinical trials
- pre-symptomatic individuals who are positive for familial MND genes (these have shown changes to personality before the development of motor changes).
The current thinking about MND is that it begins focally, then spreads along neural pathways. This
could lead to the development of regional therapy to contain the spread.
Prof Paul Talman
Australian MND Registry
What have we learned in the 14 years of the Registry?
Est 2004, pharma had deserted the field after failed clinical trials. AMNDR created to advance research.
Hope to improve patient care through observing patient management, to anticipate care needs.
Hope to meaningfully aggregate patients together so we can give them a prognosis when we first see them.
Major change is going from opt-in Registry to opt-out Registry. Opt-in is now thought to be unethical. Opt-out – unless you sign consent to get out, you’re in the Register. Very important to get a more accurate population-based analysis.
“I’m really optimistic for the future for the next 5 to 15 years… It WILL lead to a cure.”
Carol Birks
CEO, MND Australia
Our Vision: A world without MND
Our Mission: To promote, influence and advance MND care and research to improve the lives of all
Australians impacted by MND
Influencing government policy is a long-term commitment. Requires focus, flexibility, patience.
Contributed via submissions, hearings, roundtables, position statements. Collaborating with other disability organisations, Neurological Alliance Australia – joint statements and submissions.
Developed NDIS Practice Guide for MND – the first disease-specific practice guide for the National Disability Insurance Scheme (est 2008). Ten years on – people under 65 entitled to NDIS. Still advocating for older Australians to be included. Aim to end discriminatory 65 age cap, end denial of supports based on life expectancy.